Making Sense of the New Mammogram Guidelines
Ever since the American Cancer Society (ACS) issued their new Breast Cancer Screening Guidelines October 2015, my patients have been coming into my office confused about what they should do about a mammogram.
While the American Cancer Society helps so many people in so many ways, I believe they’ve done a disservice to women with their new Guidelines.
The New ACS Guidelines for Screening Mammography
The new American Cancer Society (ACS) Breast Cancer Screening Guidelines, published in JAMA, The Journal of the American Medical Association, make these changes to the existing guidelines:
1) NEW AGE TO START MAMMOGRAMS The first change is that the ACS Breast Cancer Screening Guidelines state that women should have their yearly mammogram starting at age 45—and that it is “a woman’s choice” if she wants to have a mammogram between the ages of 40 and 44. In other words, mammograms are no longer recommended and advised for women between the ages of 40 and 44.
The old ACS Guidelines recommended starting yearly mammograms at age 40.
> The ACS rationale: According to the American Cancer Society, the rationale for recommending mammograms starting at age 45 instead of 40 is this: between the ages of 40 and 45 there are a number of false positive mammogram readings, which can result in unnecessary biopsies. (A false positive is a suspicious finding on the mammogram that needs to be biopsied to determine if it is benign or cancerous, and it turns out to be benign or normal—not cancer.) Naturally, biopsies cause stress and we would like to avoid unnecessary biopsies if possible.
In addition, the ACS says that if a woman develops breast cancer—despite not having a mammogram between the ages of 40 and 44—the survival rates (whether she’s had a mammogram or not) are the same.
In other words, if we follow the new Guidelines and do not have a mammogram between the ages of 40 and 44, and we develop breast cancer, our survival rate will be the same as if we did have a mammogram. So the rationale is that if the survival rates are the same and the women who do not develop breast cancer avoid unnecessary biopsies, why have the mammogram between the ages of 40 and 44?
> Why this change doesn’t make sense: First of all, the guidelines are based on outdated technology. The new ACS Breast Cancer Screening Guidelines referred to a study, which looked at results obtained with old film mammogram technology—not the state-of-the-art digital mammography that’s available today.
“Current digital imaging reduces the false positive rate on mammograms.”
Also, outcomes are not the only factor of importance. According to the ACS, survival rates are the same for women who had a mammogram at an earlier age and for those who did not. But this does not take into account the significant treatment that a non-mammogram patient may have had to undergo to survive. Some treatments (e.g. chemotherapy) may have been avoided had the cancer been found at an earlier stage.
Looking only at outcomes—and not what the patient had to go through to achieve that outcome—is flawed, in my opinion.
2) ELIMINATING THE DOCTOR’S PHYSICAL EXAM The second change is that the new ACS Breast Cancer Screening Guidelines eliminate the need for an annual doctor physical breast exam.
The old ACS Guidelines recommended a yearly physical breast exam by a doctor starting at age 40.
> Why this change doesn’t make sense: Physical exams by a doctor can help: The elimination of the physician’s clinical exam baffles me. While the exam cannot determine if a woman has cancer, it’s a simple step that’s easy enough for a doctor to do as part of a routine physical examination. There’s no reason to skip this screening. Yes, women can—and should—be conducting home breast self-exams, but an exam by an experienced doctor certainly cannot hurt.
3) NEW RECOMMENDATIONS FOR 55+ The third change with the new ACS Breast Cancer Screening Guidelines is that women should have mammography screening every 2 years after age 55.
The old ACS Guidelines recommended women ages 55+ have screenings every year.
According to the American Cancer Society, because breast cancer in post-menopausal women tends to develop more slowly, women age 55 and older do not need to screen every year.
> Why this change doesn’t make sense: If you have breast cancer—no matter how slowly it develops—it’s still better to catch it early and treat it early, than it is to find it later and risk possibly having to undergo more invasive treatment like chemotherapy.
My Recommendations for Mammograms
Here’s my stance on mammograms—and this is what I recommend to my patients: follow the American Congress of Obstetricians and Gynecologists (ACOG) Guidelines. When the American Cancer Society Guidelines were released, ACOG released a statement that ACOG Guidelines were not being changed despite the new opinion from the American Cancer Society.
The ACOG Guidelines state that:
√ Women should have a mammogram every one to two years (I tell my patients every year is best) if you’re age 40 to 49, and then every year after that if you’re 50 or older.
Patients with a higher risk of developing breast cancer need to start their screening mammograms at a younger age than the average woman, in some cases as young as age 20. In addition, a breast MRI may be recommended.
High-risk patients include those with BRCA1/2 gene mutations, a first-degree relative with BRCA1/2 gene mutations, a strong family history of breast and/or ovarian cancer, a personal history of breast cancer, and a history of chest wall irradiation and certain syndromes such as Li-Fraumeni and Peutz-Jeghers Syndromes.
All patients are advised to discuss the timing of their mammograms with their physician.
√ Physical exams by a doctor are important, starting at the age of 18.
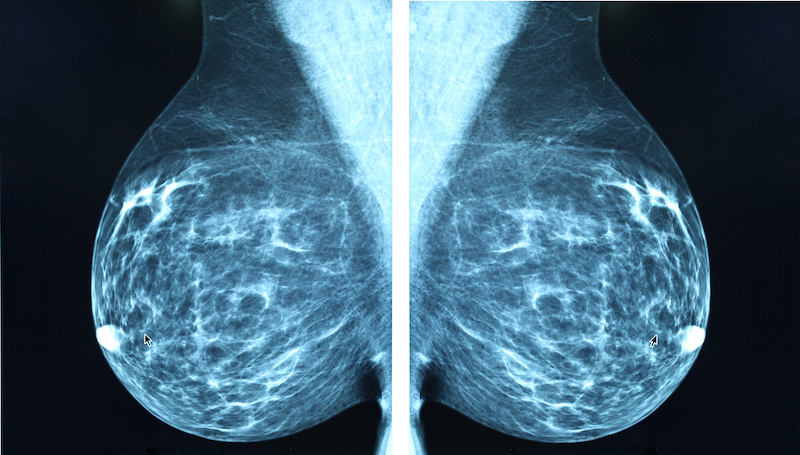
What Type of Mammogram Should You Have?
All patients are encouraged to make sure they are receiving digital mammograms (as opposed to film) if possible. Digital mammograms are especially important if you’re under age 50 and/or have dense breasts. 2D digital is readily available, and if 3D mammogram is available, this is even better.
“2D mammograms are like standard TV, while 3D is high-definition TV.”
If you have fibrocystic or dense breasts, I recommend an ultrasound with your digital mammogram.
> “Can I have thermography instead of a mammogram?” A lot of patients ask this question. Thermography is a radiation-free screening method that uses computer software to measure and compare thermal abnormalities in the breasts and create a breast “map” to look for signs of developing breast cancer. There is no compression, so thermography hurts less.
But thermography is NOT as good as mammograms in detecting early breast cancer. Up to 50% or more of cancers are missed on thermography. Thermography is not a substitute for a mammogram!
The bottom line: stick to the ACOG Guidelines—and request a 3D mammogram if it’s available. In some cases insurance will not cover a 3D mammogram, but it is well worth the out-of-pocket expense.
Back to blog